- HOME
- Department
- Hypertension & Nephrology
Hypertension & Nephrology
(1) Overview
At the Department of Hypertension & Nephrology, we diagnose and treat patients with kidney diseases and high blood pressure. Specific conditions we manage include acute kidney injury (AKI), chronic kidney disease (CKD), fluid and electrolyte imbalances, primary glomerular diseases (such as acute and chronic glomerulonephritis syndromes and nephrotic syndrome), kidney disorders caused by systemic diseases (such as diabetic nephropathy, collagen diseases, and hypertension), all types of blood purification therapy (renal replacement therapy), and both primary and secondary hypertension.
We utilize imaging studies and renal biopsies for the diagnosis and treatment of kidney diseases. For patients with advanced chronic renal failure (CKD Grade 3b or higher), we aim to slow disease progression through both outpatient and inpatient educational programs, using clinical pathways that outline a scheduled plan of care during hospitalization.
When patients with advanced CKD (Grade 3b or higher) progress to the point of requiring dialysis, our physicians take full responsibility for their care, including blood purification therapy, providing consistent, comprehensive management for each individual.
(2) Policy
Collaboration on CKD Management
Some patients referred to our department with a diagnosis of CKD may believe that the issue lies solely in impaired kidney function or the potential need for dialysis. However, this understanding does not align with the actual concept of CKD.
CKD is a concept that was proposed based on findings that individuals with kidney damage have a higher risk of developing cardiovascular diseases such as myocardial infarction. In Japan, it was previously estimated that 1 in 8 adults had CKD (*1), but recent studies suggest that the number is closer to 1 in 5, or about 20 million people (*2).
In collaboration with local clinics, we determine whether a patient’s CKD can be managed through routine health checks or if regular outpatient visits are required. We also identify the cause of CKD, assess the risk of cardiovascular events (e.g., heart attack, stroke), and evaluate the risk of dialysis initiation. Through this collaborative network, we provide community-based care for CKD patients.
CKD Education for Patients With Chronic Kidney Disease (Grade 3b and above)
Figure 1 illustrates the course of renal function decline (serum creatinine [Cr] levels) in patients who initiated dialysis at our hospital between 1991 and 1994, categorized by disease (IgAN: IgA nephropathy, DM: diabetes mellitus, HT: hypertension, PCK: polycystic kidney disease). This data demonstrates that while disease progression varies by condition, most diseases share a common pattern: a slow phase, a sudden turning point, and a rapid decline.
[Figure 1: Progression leading up to the start of dialysis according to disease]
Figure 2 shows the typical Cr levels at the transition point for each condition:
- IgAN: 2.17 mg/dL
- DM: 1.87 mg/dL
- HT: 2.59 mg/dL
- PCK: 3.09 mg/dL
We believe that delaying the time to reach these transition points helps extend the period before dialysis initiation. Therefore, we place great emphasis on blood pressure management in our daily practice.
[Figure 2: Typical Cr shifts for four diseases up to end-stage renal failure]
Hypertension Consultations
In diagnosing and treating hypertension, we focus on three main principles:
- Determine whether the patient truly has hypertension.
We encourage home blood pressure monitoring. - Differentiate between primary and secondary hypertension (hypertension with a cause).
- Prevent complications of hypertension, such as stroke, fundus hemorrhage, cardiac hypertrophy, myocardial infarction, proteinuria, and renal function decline.
- Weight Control: Maintain a BMI under 25
- Salt Restriction: Limit to 6g/day
- Consumption of vegetables (excluding patients with renal failure)
- Vegetable Intake(except for patients with renal failure)
・Men: up to 180ml sake, 500ml beer, or 2 glasses of wine
・Women: half of the above - Smoking Cessation
Blood Purification Therapy
We initiate dialysis (hemodialysis or peritoneal dialysis) for patients whose kidney function has declined significantly (CKD Grade 3b or higher). We also provide inpatient blood purification therapy for patients who are admitted for surgery or treatment but are already undergoing dialysis at other institutions.
Furthermore, we perform plasma exchange and hemoadsorption therapy for patients with neurological disorders such as Guillain-Barré syndrome, gastrointestinal diseases such as inflammatory bowel disease, or sepsis. We also provide acute blood purification for acute renal faliure and continuous renal replacement therapy (CRRT) for multi-organ failure.
(3) Departmental Characteristics
The department specializes in a wide range of conditions from preventative medicine, cancer care, to emergency medicine.
Preventive Medicine
Self-management is crucial for hypertension prevention and treatment. We encourage lifestyle modifications and home blood pressure monitoring (see Figure 3).
Lifestyle Modifications:
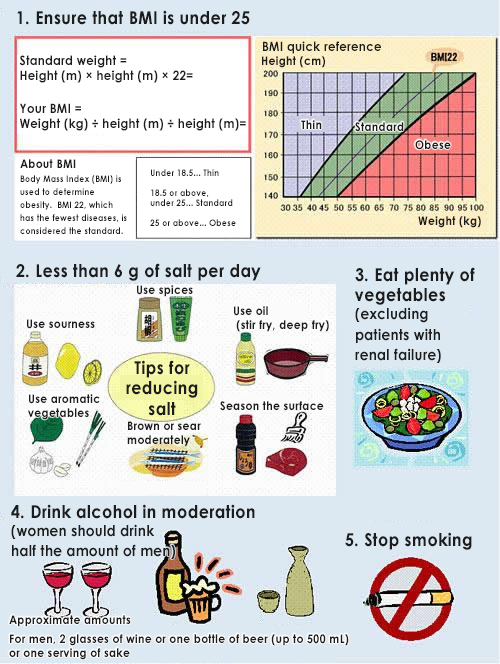
[Figure 3: Lifestyle Modifications]
Home Blood Pressure Monitoring:
We recommend twice-daily measurements (morning and evening) using an upper-arm cuff (see Figure 4). Home monitoring helps identify white-coat hypertension (high BP only at the clinic) and masked hypertension (normal clinic BP but high at home), both of which are important for proper diagnosis and treatment.
Our department has been treating hypertension for a long time based on blood pressure measurements taken at home and in outpatient clinics.
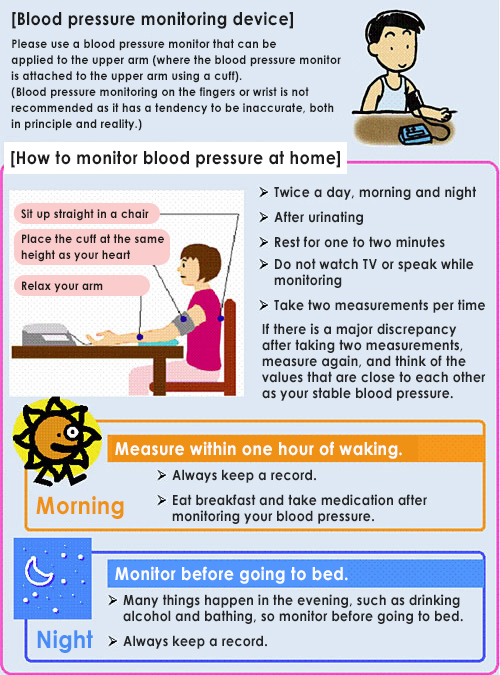
[Figure 4: How to Measure Blood Pressure at Home]
Cancer Care (Support for Other Departments)
In Japan, 1 in 2 people are expected to develop cancer in their lifetime (*3), and approximately 1 in 5 adults has CKD (*2). As a result, more patients with renal impairment are receiving cancer treatment. With increasing diversity in cancer therapies, renal complications have also become more common.
The concept of Onco-Nephrology emerged in 2011 to improve care for cancer patients with kidney issues. Our department supports cancer care across various specialties by providing nephrology expertise.
Emergency Medicine
Patients admitted to the hospital for emergency hospitalization due to severe infections or critical conditions often suffer from multi-organ failure, including the kidneys. Our department contributes to emergency medicine by providing continuous renal replacement therapy (CRRT) in the intensive care unit.
References:
1.Evidence-Based CKD Guidelines 2023 – Japanese Society of Nephrology
2.CKD Clinical Practice Guide 2024 – Japanese Society of Nephrology
3.Latest Cancer Statistics 2022 – National Cancer Center
https://ganjoho.jp/reg_stat/statistics/stat/summary.html
Related link: Hemodialysis Center