- HOME
- Department
- Cardiovascular Surgery
Cardiovascular Surgery

(1) Overview
Our Cardiovascular Surgery Department specializes in surgical treatments for heart and blood vessel diseases in adults. We are dedicated to optimizing the safety of our surgeries and actively incorporating minimally invasive heart surgeries such as off-pump bypass, stent graft interpolation, and minimally invasive cardiac surgery (MICS). We are offering a wide range of heart surgeries, except for the treatment for children and the heart transplant surgeries.
(2) Policy
We Aim to Eliminate Fear of Heart Surgery for Our Patients by Performing Minimally Invasive Surgeries
Our department is actively undertaking minimally invasive heart surgery. There are many patients who delay the timing of their heart surgery due to the fear of having heart surgeries and unfortunately missing the optimum timing for the surgery. The problem is often compounded by the fact that the symptoms of heart disease tend not to appear until the disease is severe, resulting in the surgeries being delayed even further. In order to enable our patients to have surgery at the optimum timing, the conventional fearful image of heart surgery needs to be eliminated. We seek to provide highly safe surgeries, while alleviating some of the physical and mental stress caused by the surgeries.
(3) Our Strengths
We Offer Off-Pump Coronary Artery Bypass Surgeries Without Stopping the Heart,
The heart usually pumps approximately 100,000 times per day to maintain life. Ordinarily the heart operation is performed while the heart is temporarily stopped using the artificial heart-lung machine.
With the recent advancement in surgical technologies and techniques, it has become possible to perform heart surgeries without stopping the heart or using an artificial heart-lung machine. We often perform our heart surgeries without stopping the heart to minimize the stress placed on the body.
We perform heart surgeries without stopping the heart in the cases of “coronary artery bypass surgeries” where patient’s own blood vessels as graft vessels to recover blood flow in the coronary artery. We perform surgeries for diseases such as Angina Pectoris or Myocardial infarctions. Angina pectoris and myocardial infarction are diseases where the coronary artery becomes thin or clogged due to hardening of arteries (arteriosclerosis).
Coronary artery bypass is a delicate surgery where approximately 1.5 mm blood vessels are sewn together with a thread that is thinner than a human hair, and traditionally it needed to be conducted when the heart was stopped. However, with the advances in surgical technologies, it has become possible to conduct the same quality of surgery while keeping the patient’s heart moving. We endeavor to conduct off-pump coronary artery bypass where appropriate, to minimize the stress on patients from the heart operation.
Minimally Invasive Cardiac Surgeries (Mics) Using Small Incisions

Median sternotomy

Minimally invasive cardiac surgery (MICS)
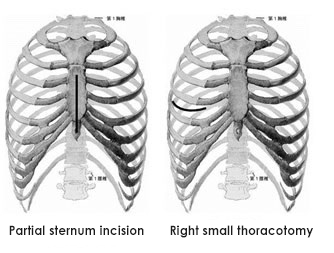
Traditionally, heart surgeries are performed using “median sternotomy incisions”, where incisions are made along the length of the sternum (a flat bone located in the center of the chest). With this method, not only would a large scar remain from the base of the throat to the stomach area, but many patients would also often struggle with pain and exercise restrictions for several months post operatively,
To improve this, we perform “minimally invasive cardiac surgery” (MICS)where no incision or minimum incisions are made over the sternum. We perform MICS for treating poorly functioning heart valves, including those that have multiple valve issues at the same time (e.g. mitral valves and tricuspid valves).
The incision size required for MICS is often less than 10 cm. We would also be able to minimize the amounts of incisions further by optimizing the incision sites depending on the positions of the heart valves and the patient’s body habitus. Although MICS requires heart lung machines to operate, MICS enables patients to make faster recovery by minimizing the incision size and the post operative pain. Minimizing the size of the scar would also have an additive benefit on reducing fear of heart surgery for our patients.
Another advantage of MICS is that there is a reduced risk of developing infection of the thoracic bones post operatively as the operation is performed without cutting of the bones. On the other hand, it is worth noting that the operation is often more challenging using this method due to a limited availability of the operative field for the surgeons.
The good news is that the cost of heart valve surgeries using MICS and the conventional sternotomy incisions do not differ significantly. If you are a Japanese medical insurance holder for example, the cost of your out-of-pocket expense is approximately 150000 yen ((If the Eligibility Certificate for Ceiling Amount Application “C” is used with the one valve replacement. This ceiling amount for the High-Cost Medical Expense Benefit System may differ depending on the patient’s income.)
*A median sternotomy heart valve surgery is approximately 140,000 yen. (If the Eligibility Certificate for Ceiling Amount Application “C” is used with a valve replacement surgery. The ceiling amount for the High-Cost Medical Expense Benefit System may vary depending on the patient’s income.)
Stent Graft Treatments, Conducted Without Cutting the Chest or the Stomach
Stent graft interpolation is a surgery conducted to treat a disease known as an aortic aneurysm where the aorta blows up like a balloon, and if left untreated, may rupture and lead to death. It is a treatment where an artificial blood vessel with metal springs called a stent graft is folded tightly, stored within the catheter and the stent is sent into the aortic aneurysm from a blood vessel via groin. The stent expands and blocks the aortic aneurysm from within once it reaches the aneurysm.
Until stent graft treatment was available, major surgery was often required where a 20 cm to 30 cm incision would have been made at the location of the aortic aneurysm. Once the aortic aneurysm is exposed, this is then resected, and an artificial blood vessel is then transplanted. An artificial heart-lung machine is also required for aortic aneurysms located in the chest area. In Contrast, the stent graft surgery, only requires a small incision (approximately 3 cm) at the groin, without cutting into the chest or the stomach. In addition, an artificial heart-lung machine is not always required for the purpose of stent surgery.
Unfortunately, not all aortic aneurysms are eligible for stent treatment. We believe that there will certainly be an expansion in the indications for stent treatments in future. We believe that there will certainly be an expansion in the indications for the stent treatments in future.
Message for Our Patients
Around the end of the 20th century, when I became a cardiovascular surgeon, both the physician and the patient believed that the cardiovascular surgeries were “the matter of life or death”. These surgeries of course continue to be treatments that are at times the matter of life-or-death situation.
By conducting the appropriate heart treatments at the appropriate time, however, the weakened heart functions can recover, and the treatment can extend the healthy lifespan even for the elderly patients. For as many people as possible to benefit from the heart surgical treatments, we need to eliminate the unnecessary fear of heart surgery. We believe that this can be accomplished not only by simply explaining the need for surgery, but also by offering surgical treatments that are less fearful.